Jugular Vein Swelling (JVD): Causes, Signs, Remedies
Jugular vein distention (JVD) is a visible bulge in the external jugular vein on the right side of a person's neck, often indicating increased pressure in the superior vena cava (SVC), a large vein responsible for transporting blood from the head to the heart and lungs. This condition can be a symptom of various underlying health issues, some of which are potentially life-threatening.
One of the most common causes of JVD is heart failure, particularly right-sided heart failure. When the heart fails to pump blood effectively, it can lead to a backlog of blood in the venous system, causing elevated JVP and JVD. Other conditions that can cause JVD include cardiac tamponade, pulmonary embolism and pulmonary hypertension, tricuspid valve disorders, tension pneumothorax, constrictive pericarditis, and infections or inflammatory conditions.
Cardiac tamponade occurs when fluid accumulates in the pericardial space, compressing the heart and impeding venous return, leading to increased JVP and JVD. Pulmonary embolism and pulmonary hypertension can increase the pressure in the pulmonary arteries, which in turn can raise the pressure in the right side of the heart, leading to elevated JVP and JVD. Tricuspid valve disorders, such as tricuspid regurgitation, can cause the right atrium to become overfilled, increasing JVP and JVD. Tension pneumothorax is a life-threatening condition where air enters the pleural space and can compress the mediastinum, impeding venous return and elevating JVP and JVD. Constrictive pericarditis, an infection of the pericardium, can prevent the heart chambers from filling up with blood properly, causing JVD. Infections and inflammatory conditions like lupus or scleroderma can also contribute to the development of JVD through mechanisms such as pericarditis.
A tumor or clot in the SVC can also cause JVD. Other risk factors for JVD include age over 65, high blood pressure, coronary artery disease, obesity, diabetes, smoking, excessive alcohol use, a high-salt diet, and low exercise levels.
Symptoms of JVD can include chest pain, shortness of breath, fatigue, palpitations, and swelling in various parts of the body. SVC syndrome, which includes symptoms like coughing, breathing difficulty, facial swelling, and lightheadedness, can also be a sign of JVD.
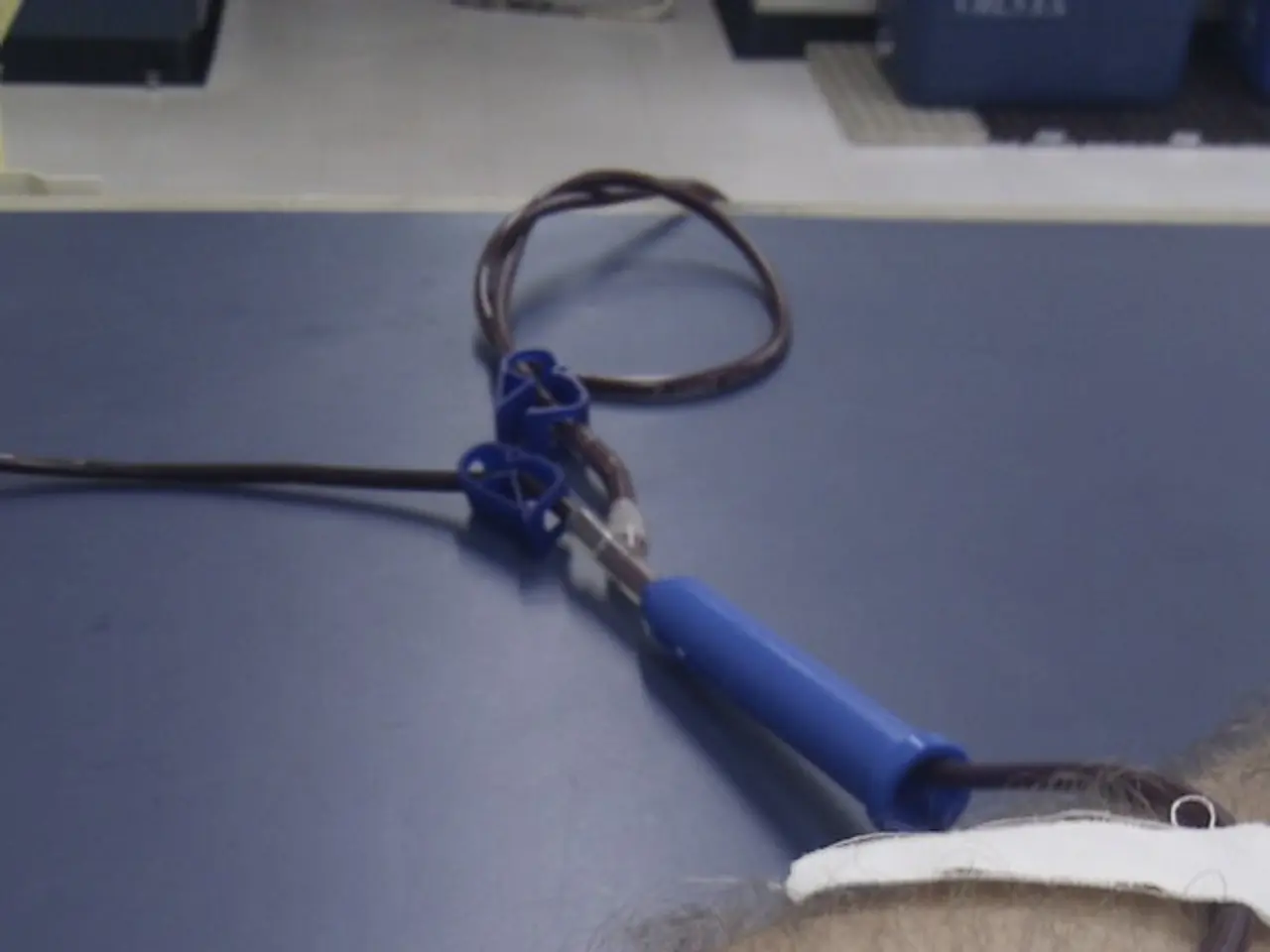
Doctors measure central venous pressure (CVP) to assess blood flow from the head to the heart and to evaluate heart health. Treatment for JVD often involves lifestyle changes, medication, and diuretics to manage symptoms and reduce the risk of complications. It is crucial for individuals to seek medical attention if they suspect they may have JVD, especially if they have risk factors for heart disease.
References: [1] Goldhaber, S. Z., & Loscalzo, J. (2018). Pulmonary embolism. The New England Journal of Medicine, 378(21), 2031-2041. [2] Yancy, C. W., Jessup, M., Bozkurt, B., Butler, J., Casey, D. E., Drazner, M. H., ... & Stevenson, L. W. (2013). 2013 ACCF/AHA guideline for the diagnosis and management of heart failure in adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation, 127(4), e344-e428. [3] Packer, M., & Tang, W. (2016). Pulmonary hypertension: current concepts and future directions. Journal of the American College of Cardiology, 67(17), 1996-2010. [4] Fang, J., & Morrow, D. L. (2015). Tension pneumothorax: the forgotten cause of death. The Journal of Thoracic and Cardiovascular Surgery, 149(6), 1829-1832.
- Additionally, ulcerative colitis, a type of inflammatory bowel disease, can potentially lead to JVD due to increased pressure in the venous system, affecting the heart's functionality.
- Macular degeneration, a common cause of vision loss in older adults, is not directly related to JVD, but it is important to note that managing health-and-wellness conditions like diabetes and cardiovascular health can reduce the risk of both JVD and macular degeneration.
- Depression and certain mental health conditions, such as bipolar disorder, can co-occur with JVD due to shared risk factors like obesity and sedentary lifestyle.
- Predictive models in science can help identify groups of people at high risk for developing JVD based on various medical-conditions and lifestyle factors, improving early detection and treatment.
- COPD, a progressive lung disease, can lead to increased pressure in the lungs and potential long-term impacts on cardiovascular health, indirectly contributing to JVD development.
- Dry eyes, a common condition affecting many people, is not directly related to JVD, but maintaining overall health-and-wellness, including cardiovascular health, can help alleviate dry eye symptoms.
- The AQ, a cognitive ability test, does not have any direct association with JVD; however, managing overall mental and cardiovascular health can increase one's ability to cope with stress and potential complications of JVD.
- While migraines are not directly related to JVD, managing cardiovascular health through lifestyle changes, medication, and regular medical checkups can help reduce the frequency and severity of migraines.
- Medical-conditions like diabetes, obesity, COPD, and mental health disorders can increase the risk of developing heart disease and, consequently, JVD; thus, it is crucial to prioritize health-and-wellness, cardiovascular health, and regular medical checkups for early detection and treatment.