The Limit Your Heart Can Endure Before Exhaustion Causes Its Demise?
Burnout, a state of emotional exhaustion and chronic stress, has been identified as a significant risk factor for various cardiovascular problems. A growing body of research indicates that burnout can lead to long-term damage to heart health, increasing the risk of heart disease, hypertension, arrhythmias, and metabolic issues.
The link between burnout and heart health is largely due to the chronic elevation of stress hormones like cortisol and adrenaline, which keep the cardiovascular system in a constant state of overdrive. This sustained stress response can cause arterial damage and promote inflammation inside blood vessels, worsening cardiovascular health.
One of the most concerning aspects of burnout is its ability to trigger arrhythmias, causing irregular heartbeats and palpitations, which may become chronic with ongoing burnout. Additionally, burnout can contribute to metabolic disturbances such as high cholesterol and blood sugar levels, both key risk factors for heart disease.
Moreover, burnout often leads to persistent high blood pressure, further straining the heart and blood vessels. This continuous stress can also fuel poor lifestyle habits such as unhealthy diet, lack of physical activity, smoking, and alcohol use, which add to heart disease risk.
Furthermore, chronic stress weakens immune function and increases inflammation, which negatively affects cardiovascular health and recovery from heart-related problems. Psychologists have found that thoughts, perfectionism, and emotional suppression, common in burnt-out individuals, can worsen the body's stress response.
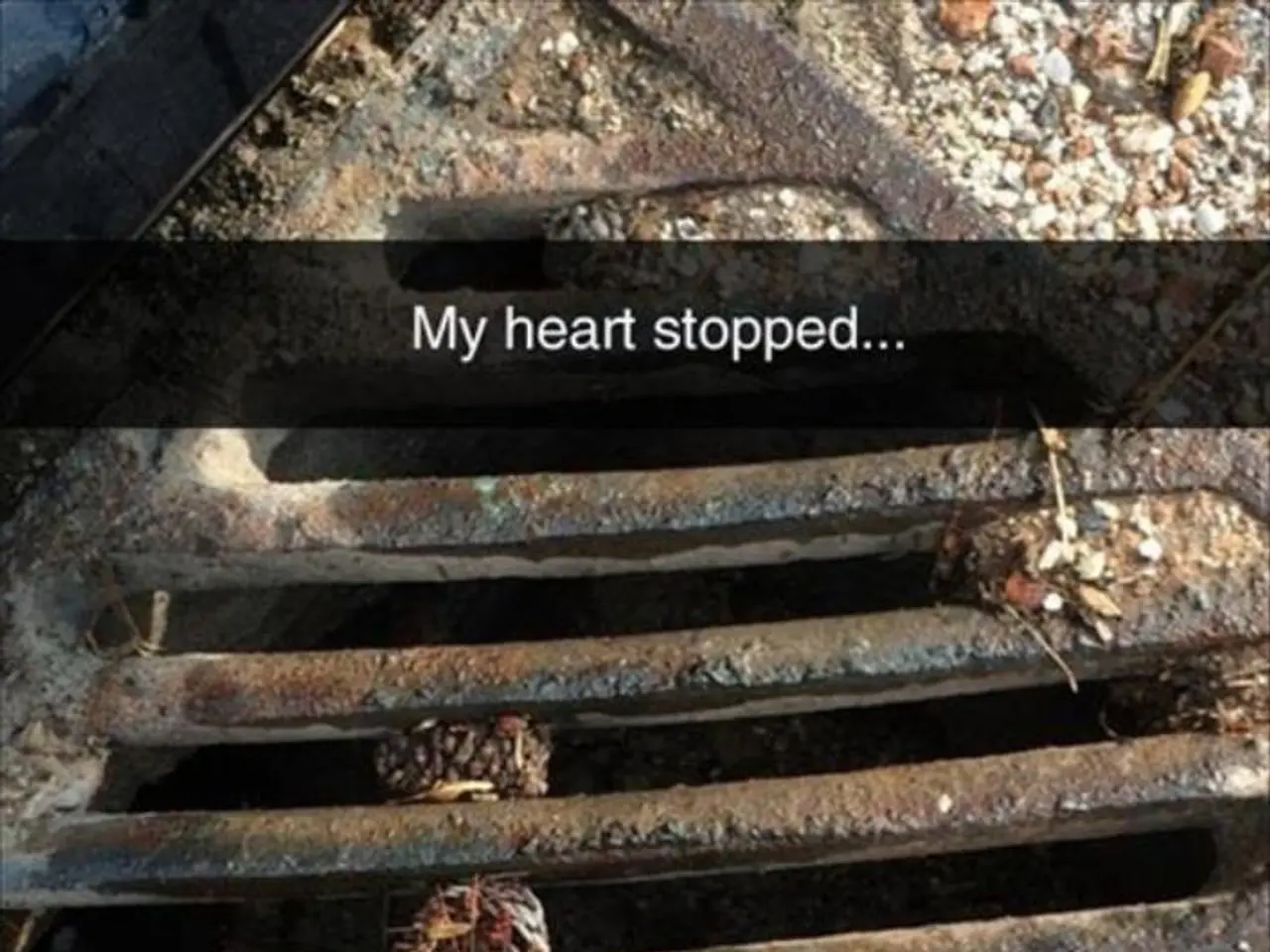
It is essential to note that the emotional suffering of burnout is often dismissed until the manifestations appear to be inescapable. Burnout's cognitive symptoms often precede its physical ones, with signs such as persistent fatigue, aversion to people or work, lack of emotion, and trouble sleeping. Other physical symptoms may include chest tightness, abnormal heartbeat, breathlessness, dizziness, lightheadedness, continually occurring stomach issues, or migraines. These symptoms indicate that the mind-body system is being attacked, not mere "symptoms of stress."
With early intervention, rest, therapy, and lifestyle changes, both mental and heart health can improve. Prioritizing healing and mental recovery can dampen the activation of the HPA axis, a core stress-response system. Engaging in Cognitive Behavioral Therapy (CBT) or mindfulness practices can help reprogram the mind, cultivate emotional resilience, and establish homeostasis in the body.
Seeking help from an appropriate teacher, peer, or therapist can offload emotional burdens before they develop into physical pain. Burnout, initially described by Freudenberger in 1974, consists of three core symptoms: depersonalization, emotional exhaustion, and reduced personal accomplishment.
Burnout is more prevalent in individuals with high-stress jobs, little control over work-life balance, or those who provide care, such as physicians, CEOs, nurses, teachers, and parents. Burnout is caused by extended periods of unchecked stress exacerbated by inadequate recovery. It is crucial to address burnout not as a personal failure but as a serious message that system changes are urgently needed.
In conclusion, burnout poses a significant threat to heart health, causing enduring physical changes that can silently deteriorate heart health over time. Early awareness and lifestyle changes are critical to mitigating these risks.
Mental health professionals should prioritize identifying burnout in their clients, as it can lead to long-term damage to heart health and increase the risk of heart disease, hypertension, arrhythmias, and metabolic issues. The science behind heart-and-wellness reveals that burnout often triggers arrhythmias, persistent high blood pressure, and metabolic disturbances, all major risk factors for heart disease.